Simon Stevens, the NHS England Chief Executive, just told the Public Accounts Committee that some Sustainability and Transformation Plans will soon get going as Accountable Care Organisations or systems.
This sounds like more tedious, senseless jargonising.
Indeed one MP, Anne Marie Morris, was so bemused by what Simon Stevens was saying, she asked if they were all smoking dope.
But behind the jargon smokescreen – whether wacky baccy or not -setting up Sustainability and Transformation Plans to run the NHS as Accountable Care Organisations opens up the NHS to privatisation on a bigger scale than anything seen so far.
And it is a mechanism for limiting the range of care that the NHS offers, and for denying care to patients who are judged to offer poor value for money.
This would mean the end of the NHS as a service that provides the full range of health care to anyone who has a clinical need for it.
How does this work?
Sustainability and Transformation Plans require the speedy dismantling of the NHS to turn it into a health service that is based on the US Medicare model – a limited publicly funded/privately provided health insurance scheme for people who are too poor to pay for private health insurance. Key Medicare providers include United Health, the former employer of Simon Stevens, now NHS England’s Chief Executive.
Sustainability and Transformation Plans copy Medicare’s “new models of care”, that are delivered through:
- a “modern” – ie de-skilled and de-professionalised (cheaper) – workforce,
- lots and lots of costly digital technology and
- new types of contracting that involve setting a fixed per person budget for a population, instead of the current payment per treatment.
This bulk contracting with a fixed per person budget (aka capitated budget) restricts patients’ access to limited treatments, that are specified as “managed care pathways.”
It also contains an incentive to limit care to patients who are cheapest to treat and offer the best return on investment. Providers are allowed to keep any “profit” – and they carry the risk of overspending.
Responsibility for carrying the risk of overspending has already led to the collapse of one of the first NHS Accountable Care Organisations, the Torbay and South Devon Integrated Care Organisation – see below for more info.
These limitations on the types of care and restrictions on who gets care -aka “demand management” will drive people who can afford it, to go private.
Such bulk capitated contracts are also probably unlawful, under current NHS legislation.
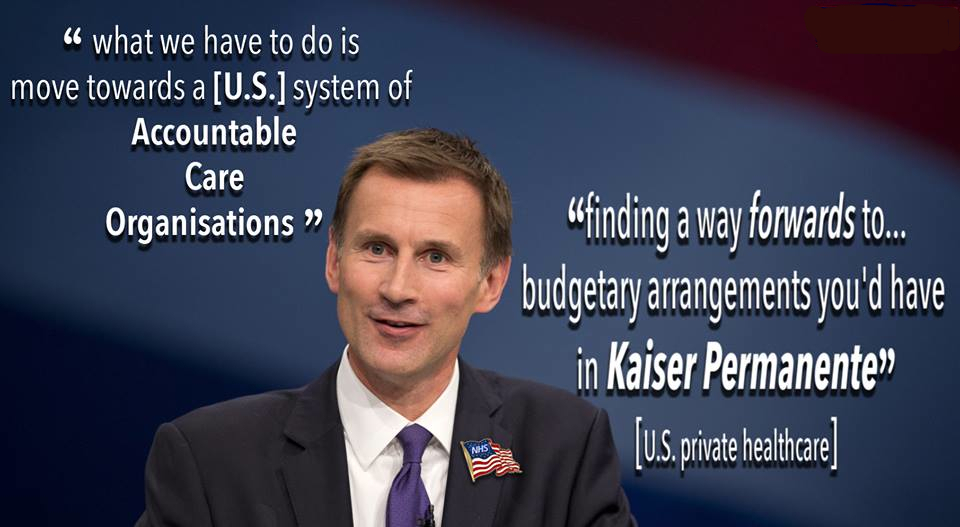
That does not deter Simon Stevens, who on 27th February told the Public Accounts Committee:
“We will get probably between six and 10 of them [STPs] going as accountable care organisations or systems, which will for the first time since 1990 effectively end the purchaser-provider split, bringing about integrated funding and delivery for a given geographical population. This is pretty big stuff, and people are pretty enthusiastic about it.”
The Public Accounts Committee were not so enthusiastic, since they’d just spent ages questioning Simon Stevens and other key NHS and social care bureaucrats about the National Audit Office report on the failure of integration of health and social care through the Better Care Fund.
MPs described the situation as chaotic.
Ending the purchaser/provider split locks in large-scale privatisation
Ending the purchaser/provider split in a marketised/privatising NHS is a sly way of locking in privatisation on a scale we’ve not seen before – as planned by the previous NHS England boss David Nicholson and reported by Alex Nunns in 2013.
- You start out with an integrated NHS that is one of the most efficient in the world.
- Then you split the purchasers from the providers, as the Tory government did around 1990.
- Then you privatise the providers. As the New Labour, Coalition and current Tory government have.
- Then you privatise the purchasers. As the current Tory government has.
- And then you set up ACOs (aka Integrated Care Organisations) to abolish the purchaser provider split!
Except in the meantime you have successfully moved a public health service into the private sector. And in just four simple steps!
The recent King’s Fund’s Sustainability and Transformation Plan Report claims that doing this would require legislative change, to remove the competition requirements of the 2012 HSCA. Such legislative change would lock in NHS privatisation.
The kind of legislative change the Kings Fund is talking about would be like the Efford Bill, which the Labour Party put forward as an alternative to the NHS Reinstatement Bill, to take out the competition section of the HSCA.
The trouble with this is that once you remove competition from a marketised NHS, you allow private health companies to establish monopolies.
All the pieces for terminal NHS privatisation are being stealthily manoeuvred into place. And campaigners are being diverted from these machinations by a mega march calling for an end to NHS under-funding. Which wouldn’t solve these problems at all.
It would create a bigger income stream for profiteering private companies that are manoeuvring – with government support – to take over the NHS.
Pro-privatisation think tanks spread misinformation for governments
The promotion of Accountable Care Organisations that replicate US private health insurance models is based on “evidence” that comes from the pro-privatisation think thanks and management consultants that the Department of Health and NHS England have effectively outsourced policy making to. Their suggestions are built on sand.
George Monbiot’s analysis of the role of lobbyists and consultancy companies in spreading the misinformation ocean that Donald Trump floats in also applies to successive governments’ stealth plans to dismantle the NHS.
First wave Accountable Care Organisations are stalled
There’s no evidence that these footprint-wide Accountable Care Organisations are going to work – the Torbay and South Devon Integrated Care Organisation has already gone belly up (see below) and the Northumbria Accountable Care Organisation, aka Northumbria Healthcare, has had to delay its launch due to Northumberland Clinical Commissioning Group being broke and subject to pressure from NHS England to cover up that fact.
The poster child for NHS accountable care organisations, Northumbria Healthcare is intended to hold a single contract for acute, mental health and community services, and adult social care.
Due to go live on 1st April 2017, after operating in shadow form in the 2016/17 financial year, its launch was delayed indefinitely because Northumberland Clinical Commissioning Group – the primary commissioner for the Northumbria accountable care organisation- was broke.
Northumberland Clinical Commissioning Group’s governing body papers said the Clinical Commissioning Group required written confirmation from NHS England that its financial position would not impact on its ability to “become part of” the Accountable Care Organisation, but the NHS England quango had not made a decision yet.
The Minutes of the 26th Jan 2017 Audit Committee show that NHS England tried to get them to cover up their dire £41m projected deficit for 2016-17 – which had ballooned from the Clinical Commissioning Group’s official forecast at the end of December, of a £5m deficit for the financial year.
The Audit Committee Chair reported that at the January Joint Locality Executive Board:
“There was discussion regarding the continued formal reporting of a £5million deficit when the actual position is £41million. The CCG has repeatedly discussed the actual financial position with NHS England but has been asked to continue to report the deficit as £5million. This is a risk in terms of accurate audit trails as there are no formal minutes of the discussions with NHS England.”
(Update 10 May 2017: The 19 April 2017 Minutes of the Northumberland Clinical Commissioning Group Governing Body record that – notwithstanding the events related above – the Clinical Commissioning Group entered a period of transition on 1 April 2017, to enable the ACO to go live at a future date.
“From 1 April to 30 June 2017, the CCG, Northumbria Healthcare NHS Foundation Trust (NHCFT) and primary care (as core members of the ACO) will form an ACO transition board to manage the operational transition to the ACO (subject to approvals).”
- The Clinical Commissioning Group is in special measures with NHS England, who have “created support by appointing experts” in contract management etc. – ie parachuted in their own people to make the changes they want
- The Accountable Care Organisation business case continues to be considered by NHS England and NHS Improvement and it was now unlikely that the Accountable Care Organisation would be established before April 2018.
- With the establishment of the Accountable Care Organisation, the Clinical Commissioning Group would continue to be a statutory body and would have a contract with the Northumbria Hospitals trust that would host the Accountable Care Organisation. Boundaries between the CCG and the host hospital trust “would need to be very clearly defined in order to identify liability of any future fraud cases.”
South Devon and Torbay Integrated Care Organisation kicks the bucket
The Torbay and South Devon Integrated Care Organisation was set up in October 2015, following participation in the NHS Kaiser Beacon programme – a pilot to introduce the system used by US private healthcare company Kaiser Permanente, with the aim of cutting costly hospital services and replacing them with a new, low-cost system of integrated health and social care in the community that’s intended to keep people out of hospital. It’s known as “demand management”.
The Integrated Care Organisation’s mission was to pool health and social care budgets and run the services from under one roof – effectively the MultiSpeciality Community Provider model that is a common feature of Sustainability and Transformation Plans.
But Torbay and South Devon NHS Foundation Trust has now told the two councils involved in the Integrated Care Organisation that it is withdrawing from a ‘risk-sharing’ agreement, which splits liabilities for unexpected costs.
Torbay Council papers indicate that the Integrated Care Organisation has overspent by £12m in its first year, sparking fears that the organisation presents a ‘substantial financial risk’ to the local authority.
With financial strife in the Integrated Care Organisation, councillors have called for ‘a different dialogue’ with the Government.
No evidence this model works
This is unlikely to be a one off – as a recent BMA article reiterates , there is no evidence that this model works. Slaves to zombie policies should take note and stop cutting our hospital beds and trying to turn the NHS into a version of US Medicare complete with American health companies, and take note of the BMA article that says:
“We have the evidence problem—there is very little of it to support the idea that providing alternative service delivery models will enable more bed closures. A series of systematic reviews carried out by the Universities of Bristol and Cardiff showed very inconsistent evidence of interventions intended to prevent unplanned adult admissions to hospital. And an equally thorough review of approaches by the Nuffield Trust—including case management, integrated community teams, virtual wards, or telecare—was unconvinced of the evidence base for these interventions reducing hospital activity or bed occupancy.”
The Prime Minister, Teresa May, has announced a review of policy on social care funding, delivery and integration with health, amid huge concern about failure in the sector.
Find out more:
Here is the Public Accounts Committee oral evidence 27 Feb 2017

Brilliant!
Thanks.
Shared!
LikeLike
I work at Torbay … it’s not the system it’s the executives . Under qualified dreamers who take £1.8 million pounds to keep them comfortable and simply unable to direct or manage .
LikeLike
[…] Clinical Commissioning Group ‘light’ functions are when the Clinical Commissioning Groups slim down and their commissioning duties are subsumed into an Accountable Care Organisation or Organisations, as these organisations have commissioning powers – as in closing the purchaser provider split. […]
LikeLike
The end is coming .. private companies will soon take over our NHS .
LikeLike
Let’s not be so fatalistic – we can and will stop this if we put our minds and determination to it.
LikeLike
Terrific diatribe. Well done. Let’s see what happens after the March today. We do need a revolution you know, not just of the NHS but against the entire Parliament, which is killing the best of British – the natural generosity, the communities, the pride in being a country of the best democratic ideals, with a canny sense of right and wrong.
These people in Westminster do not represent the British. Get rid…..
LikeLike
Why does no one EVER mention the Privatised Profiteering Parasites, who sit back and let the loot from ruinous PFI contracts roll in? Cupid set the precedent with Junior Doctors – rip them up, and start again.
LikeLike
[…] [Here is a post on these devious plans]: https://calderdaleandkirklees999callforthenhs.wordpress.com/2017/03/01/wake-up-to-the-accountable-ca… […]
LikeLike
[…] up NHS privatisation and create a two tier health service by turning the NHS into a version of the US Medicare/Medicaid for patients who are too poor or ill to get private health […]
LikeLike
[…] carry out around £24bn of cuts by 2020/21 and redisorganise the NHS into local services that copy public/private partnership models like Medicare/Medicaid in the USA and the Alzira system in […]
LikeLike